Health plans are constantly changing the rules
Organizations are seeking innovative methods to reduce revenue leakage and safeguard their earned revenue.
Adopting technology, improving processes, and engaging with payers can help organizations stop revenue leaks and build a stronger financial foundation.
We can help you accelerate your revenue recovery strategy.
- Collabortive Workflows
- Revenue Integrity Solutions
Innovative methods are needed to reduce revenue leakage and safeguard revenues earned
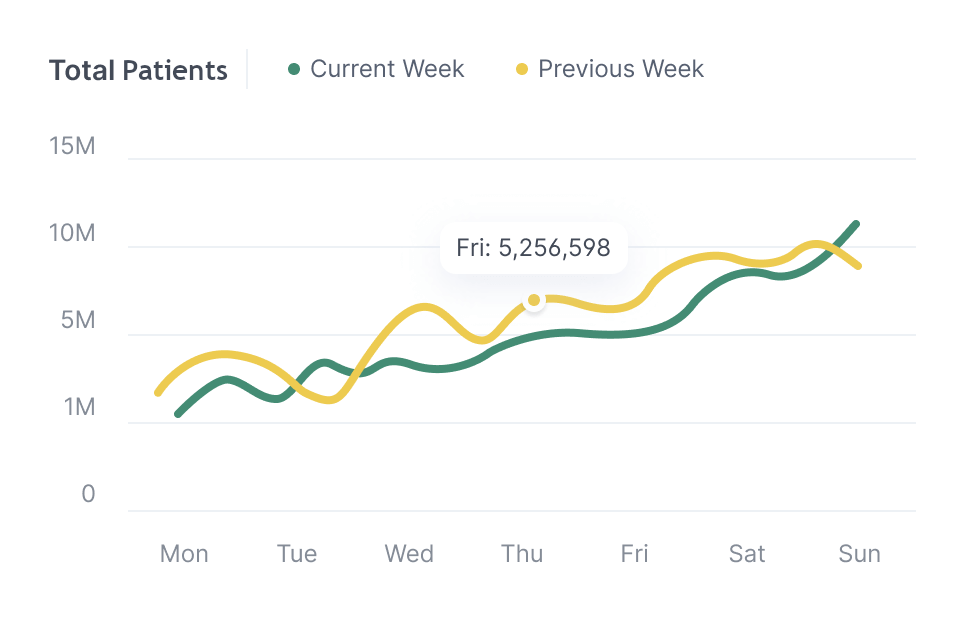
Denial Rates are on the Rise
Denial rates are now averaging 12-13.9%, a concerning trend that can impact revenue cycles and cash flow stability.
Increasing Underpayments
Claims are underpaid by an average of 9%, which can compound financial strain, especially for smaller providers or those with thin margins.
Continous Nonpayments
18% of all claims are never paid, resulting in a direct loss of revenue. This can be due to various reasons such as coding errors, lack of follow-ups, or payer policies.
Benefits of
working with us
We take a practical approach to revenue integrity
A practical approach to revenue integrity focuses on ensuring accurate billing, compliance, and efficient processes. It involves clear workflows, auditing real time contract performance to prevent revenue loss.
We know what works
To effectively detect revenue leakage from underpayments in real time, we automatically review every claim and remit for contract compliance. When discrepancies are found, we promptly and automatically appeal claims that fall short of contract fee criteria.
We support Coding and Billing
Supporting many different workflow needs...whether it is post-visit, or historical claim resolution. We do this through the detection, resolution and tracking of:
- Underpayments
- Nonpayments
- Denials
- Value Based Care
And most importantly...we support tracking, reporting, and managing Payer Contracts in real-time.
Finally, we are obsessed with our clients
We’ve all experienced difficulties with working with Payers, and our goal is to balance the scales in the Provider's favor while leveraging the most out of your contracts.
Our Platform Benefits
Simplified
Make your revenue recovery activities actionable and meaningful within days versus months.
By leveraging the existing claims sent to the clearinghouse, we can help you stop revenue leakage immediately.
Benchmarking
Easily identify interdependencies between denials and payer contract mistakes to proactively prevent revenue leakage.
Close the financial gap between those interdependencies to reverse negative leakage trends effectively.
Understanding your ROI
Contracts and payer denial behaviors are critical to assessing financial performance and strategically positioning for future success.
Advanced contract management software helps you maximize the revenue you've earned and position your organization for future success.
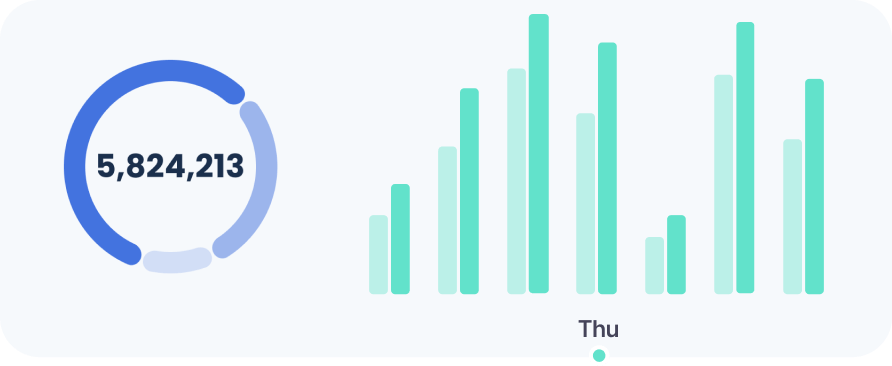
Revenue Leakage Detection and Denial Management System
Combining all aspects of contract compliance, payment tracking, data analysis, and automated appeals generation.
How does it work?
Revenue Leakage Detection
- Digitizing contract terms to manage all aspects of revenue integrity.
- Payment monitoring of incoming claims against contract terms and automatically flag any discrepancies, underpayments, or instances where the payment falls below expected thresholds.
- Real-time notifications available to managers or finance team memebers.
Automated Appeal Creation
- Once a gap in payment is detected, the system would automatically generate bulk appeals based on contract fee schedule.
- Automated drafting of appeal letters with specific comment language for discrepancies in payments or denials.
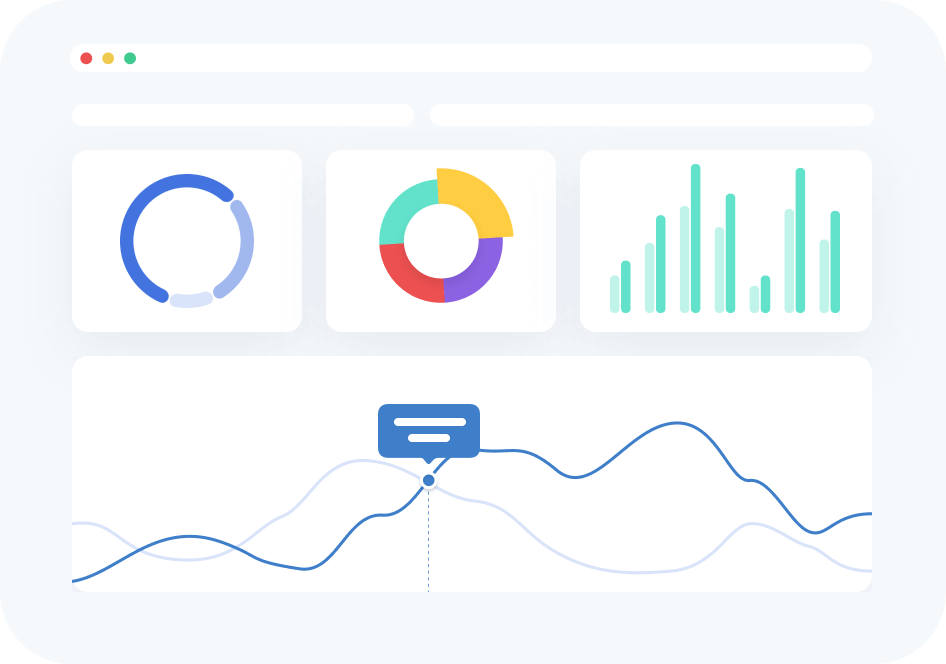
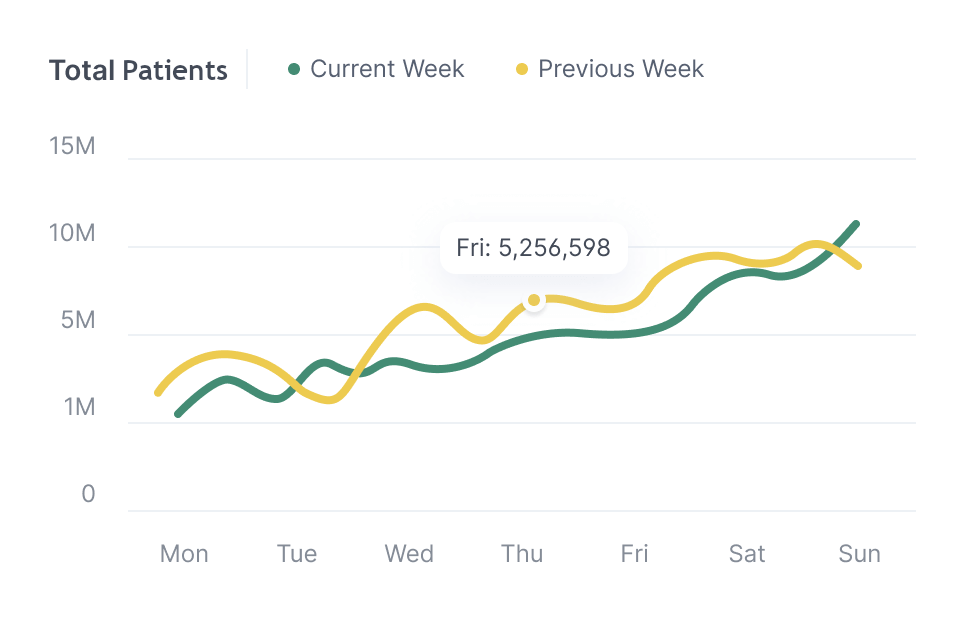
Advanced Analytics with Reporting and Dashboards
Identify and medigate payer trends in advance to immediately impact the financial health before they become a huge burden.
Get connectedMaximize your investments
with simple integration tools
Many of the best EHR and RCM companies are already capable of leveraging our solutions out of the box. We connect with many other data sources to help you get more done.
Let's talk integrationTransform your organization's revenue recovery efforts today
Stop revenue leakage today with your No-Risk trial. Integration takes less than a week.